Smart Health Data
Medicine has not escaped the influence of digitalisation. Patient data has long since been collected and evaluated in order to personalise and improve patient care using artificial intelligence (AI). In Bochum, the fields of science, business and patient care are working together on this. “Smart Health made in Bochum” projects have been developed, making the city one of the leading locations for the medicine of the future in Germany.
Deep Learning for Cancer and Alzheimer’s Research
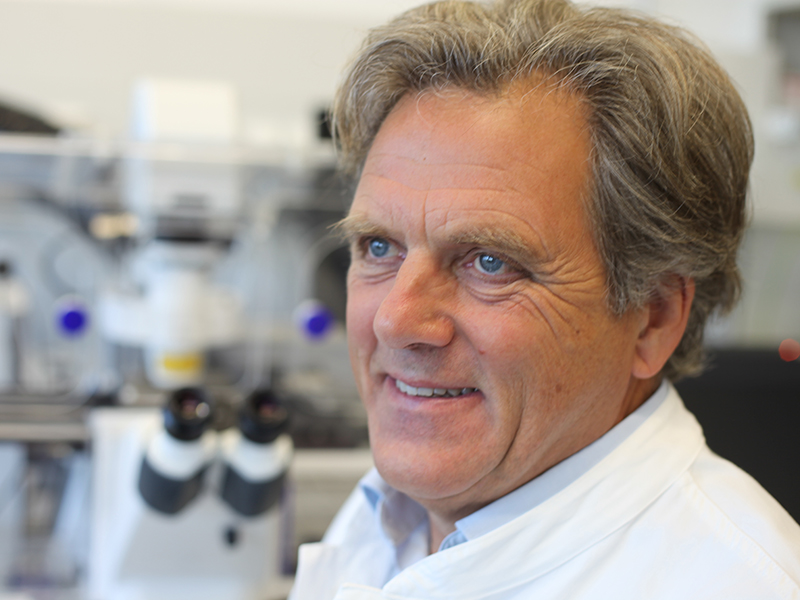
Deep Learning is a modern approach that turns Big Data into Smart Data so it can be used for the medicine of the future. It could represent a major step forwards for the diagnosis of cancer and Alzheimer’s. Prof. Klaus Gerwert from the Protein Diagnostics Centre (ProDi), for example, has been able to develop a blood test that using protein biomarkers to precisely detect Alzheimer’s up to 14 years before clinical manifestations. Prof. Gerwert is the founding director of the centre, which opened on the Bochum Health Campus in June 2019. In the ProDi research building, which has received national and state funding, around 150 scientists work on refining the early diagnosis of cancer and neurodegenerative diseases like Alzheimer's using newly developed methods of protein research. The discovery of new protein biomarkers is one of their key objectives.
Info
In Germany alone, some 1.7 million people currently suffer from a form of dementia. Predictions suggest that this number will increase to 3 million by 2050. The most common form of dementia, found in two thirds of cases, is Alzheimer’s. Roughly 15 years before the clinical manifestation, protein misfolds are observed. These then lead to the plaque formations in the brain that are typical of Alzheimer’s.
ProDi researchers are on a particularly promising path in the field of cancer diagnostics. One innovative diagnostic approach that has been developed here is “label-free digital pathology”, where a computer is used to stain diseased tissue virtually with millions of infrared spectra. So “Big Data” becomes “Smart Data” and cancer can be diagnosed precisely.
A team of bioinformatics specialists assess the infrared spectra using Deep Learning algorithms in the in-house ProDi computer cluster. The approach has already been successfully established in colorectal cancer and is currently being applied to lung and bladder cancers.
Deep Learning is applied differently in Alzheimer’s research, as testing focuses on bodily fluids, with narrower spectral bands, rather than location-specific tissue samples. Intensive work on these new approaches to the analysis of bodily fluids using biomarkers is currently being done at ProDi. Prof. Klaus Gerwert calls this “a vision of the future”. But he is certain that within a few years, thanks to Smart Health Data deployed as the Alzheimer’s blood test, Alzheimer’s will not be curable but will have been reduced to a chronic disease like HIV.
Sepsis Research in Bochum
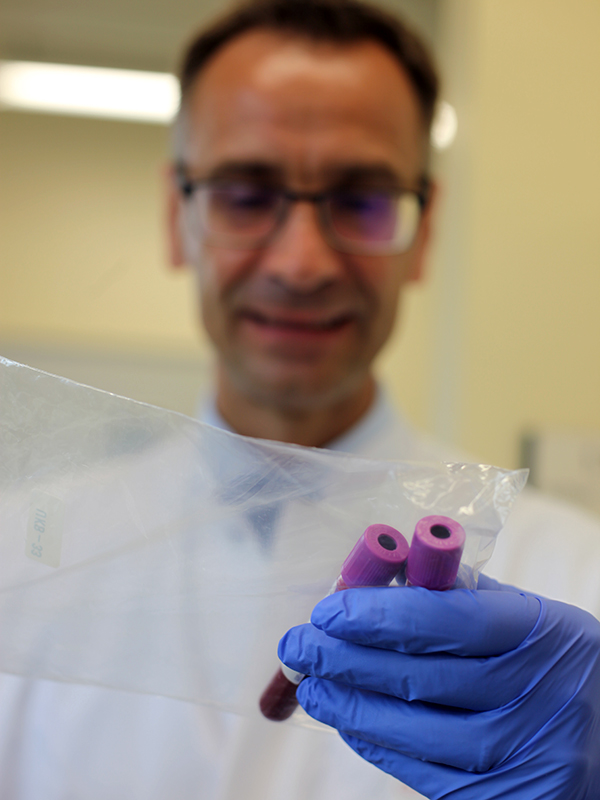
Sepsis research also places high hopes on digitalisation, with the aim of developing effective treatments and targeted patterns for investigation in the future. Today, 162 people die every day from sepsis in Germany alone. Traffic accidents kill only nine. Also called blood poisoning, sepsis is thus the third most common cause of death in Germany. Until now, the disease has not yet been investigated in depth. Despite billions in funding, almost one in two patients still dies as a consequence of sepsis. The SepsisDataNet.NRW project, funded by the state and the ERDF, has now brought together eleven funded partners and two associated partners from research, business and patient care. The objective of this project is to construct an extensive biomaterial database to identify biomarkers as a basis for diagnosing sepsis and to develop a decision support module for treating doctors.
“Quite simply, the problem is that we still don’t understand how to stop sepsis.”
Prof. Dr. Michael Adamzik, Director of the Clinic for Anaesthesiology, Intensive Care Medicine and Pain Therapy at Knappschaft University Hospital, Bochum.
The generation and evaluation of pseudonymised clinical data from currently 300 patients takes place almost every second. This means that from the first day, it is possible to predict which patients have a high probability of death. Identifiable patterns could provide researchers with the answer to successful treatment as quickly as possible and the development of drugs.
To date, eight clinics in Bochum are involved in SepsisDataNet.NRW. They provide data from digitalised patient records. As part of the follow-up project, Symbara, system medicine-based personalised sepsis analysis will be expanded from Bochum to a wider area, in order to carry out a targeted search for patterns using Big Data and AI, taking sepsis research in Germany in a completely new direction. Bochum-based KAIROS GmbH is heavily involved in both projects and makes the collection and comparison of all data possible.
Furthermore, research data is also collected from genomics, proteomics and other sectors of modern biology and medicine (Omics) for evaluation and analysis with the help of KAIROS. In order to be able to exploit this, in combination with data from hospitals, using AI, the data must be extracted from the systems and “shaped”. In other words: “They have to be translated into the same language”, explains Dr Christian Stephan, Managing Partner of KAIROS GmbH. To do this, KAIROS uses ETL processes.
Info
The words Omics comes from Greek and means “a totality”. The neologism comprises all subsectors of modern biology and medicine that end in -omics. This includes genomics, proteomics, metabolomics and transcriptomics. In medical research, this means that the totality of a set of proteins or a gene, for example, within a cell, organ or organism at a specific point in time is studied. The objective is to be able to study and analyse diseases in detail on the basis of changing processes.
“Bochum is a melting pot for a smart health digitalisation strategy. The GesundheitsCampus Bochum Agency has brought together the players and created an environment in which even new companies can be part of this network.”
Dr. Christian Stephan, Managing Partner of KAIROS GmbH
The mass of data collected and transformed by KAIROS GmbH makes it possible to develop a decision support tool. This should not replace doctors, but help them in making decisions. The close collaboration between research, business and patient care thus prepares the way for better diagnostics and care, with the objective of personalised medicine at some point.
Artificial Intelligence in Clinical Routine
Hospitals in Bochum have already started using Smart Health Data in patient care. One example of this is AI-supported diagnostics in the field of neurodegenerative diseases. At the Katholische Klinikum in Bochum, work is being done to lighten the load on doctors through computer-assisted diagnostics with MRI, CT and x-ray findings. With multiple sclerosis, for example, AI supports the preparation of data and makes the progression of the disease visible. When correlated with other characteristics and treatments, this leads to individual, personalised treatment.
Thanks to its high-performing university hospitals and leading IT and medtech companies, Bochum offers a significant network structure for the development of interdisciplinary projects and innovative products for Smart Health Data. The next step involves exchanging data between hospitals and doctors’ practices.
“Data protection is of the utmost importance when it comes to medical data."
Prof. Dr. med. Christoph Hanefeld, Managing Director of the Katholische Klinikum (Catholic Hospital) in Bochum
As part of the Falko project, radiology data is already exchanged between hospitals in the Ruhr area with no data loss. A follow-up project now aims to cover the exchange of other data, such as test results, laboratory values and cardiology data. This data transmission infrastructure means that, for example, duplicate tests and reports are avoided, and thus no longer lead to a loss of time and quality.
Info
Personalised, or individualised, medicine is based on new knowledge of molecular processes in a person's life. The progression of a disease is affected by individual factors such as genetics, lifestyle, age and sex. Science and research are working - in some cases with AI - to make these factors visible and exploitable for customised prevention, diagnosis and treatment.
“In Bochum, research is already being applied in practice.”
Prof. Dr. med. Christoph Hanefeld, Managing Director of the Katholische Klinikum (Catholic Hospital) in Bochum
Would you like to know more about what Bochum has to offer?
Give us a call!

